Comprehensive Guide: Managing Epileptic Patients Safely in Your Dental Clinic
That nagging worry creeps in—what if I have a seizure during my dental appointment? Or maybe you’re a caring family member, anxious about bringing your loved one with epilepsy in for much-needed dental work. Perhaps you’re a dental professional who truly wants to do right by every patient, no matter their medical history. The good news? With the right preparation, knowledge, and a good dose of kindness, everyone can feel confident and safe in the dental chair.
Whether you’ve lived with epilepsy for years or you’re preparing to care for a patient or loved one, you’re in the right place. This guide cuts through the tough words, breaking down how to handle dental care with epilepsy—step by step. You’ll get practical tips, real-world advice, and the support you need to make your next visit, or your patient’s, a good experience.
In This Article: What We’ll Cover
- Understanding Epilepsy and Its Dental Implications
- Pre-Appointment Preparation: Ensuring Patient Safety and Comfort
- During the Appointment: Proactive Management and Prevention Strategies
- Managing a Seizure in the Dental Clinic: Emergency Protocol
- Post-Appointment Care and Long-Term Oral Health Management
- Staff Training and Clinic Preparedness: Building a Confident Team
- Conclusion: Prioritizing Safety, Compassion, and Comprehensive Dental Care
Understanding Epilepsy and Its Dental Implications
What is Epilepsy? A Brief Overview of the Condition
Epilepsy is a brain disorder where your brain’s electrical signals sometimes go wrong, causing regular seizures. It’s more common than you might think. According to the CDC, about 1 in 26 people in the US will develop epilepsy at some point. That’s millions, both adults and kids, around the world.
Seizures don’t look the same for everyone. Some people lose awareness and just “stare off” for a few seconds (called absence seizures). Others have strong shaking and jerking—what’s often shown in movies—known as tonic-clonic or “grand mal” seizures. Triggers can be flashing lights, stress, or even being tired.
Common Types of Seizures and Their Clinical Presentation
As a dental worker or a patient, knowing what kind of seizure is happening is important. Here’s the simple breakdown:
- Tonic-clonic seizures: Full-body shaking, passing out, and possibly falling down.
- Absence seizures: Person seems to zone out or stare blankly for a short time.
- Partial (focal) seizures: Only one part of the body moves oddly or feels weird; person may be awake or not.
Different seizures mean different dangers during dental care, so always give a full health history and ask questions if you’re not sure which type you or your patient has.
Antiepileptic Drugs (AEDs) and Their Key Oral Side Effects
If you take medicine for epilepsy, you’re not alone. These drugs, called antiepileptics, do a lot to control seizures, but they can cause some problems for your mouth.
Gingival Hyperplasia (e.g., Phenytoin-induced)
This big term just means swollen, thickened gums. About half of people taking phenytoin (a common epilepsy drug) get some of this problem. Other drugs like carbamazepine or valproate can also cause it, just not as often.
When gum tissue grows over teeth, it traps germs, makes brushing hard, and ups your chance of infections and cavities.
Xerostomia (Dry Mouth)
Many epilepsy drugs, like carbamazepine and phenobarbital, can dry out your mouth. Saliva isn’t just for comfort—it helps protect against cavities and gum disease by washing away food bits and germs. Less spit means you could get bad breath, sores, and, yes, more cavities.
Increased Cavity Risk
With dry mouth and sometimes trouble brushing or flossing, it’s easier to get tooth decay. Some epilepsy meds in syrup form (often given to kids) contain sugar, which can add to the problem.
Impact of Epilepsy on Oral Health: Beyond Medication
Epilepsy isn’t just about drug side effects. Think about mouth injuries—falls or jaw clenching during a seizure can crack teeth, cut gums, or even break bones. Some folks have trouble brushing and flossing as well, making daily cleaning harder.
Research shows people with epilepsy are more likely to have gum disease, cavities, and damaged teeth. But don’t lose hope—knowing this helps us stop problems before they start.
Pre-Appointment Preparation: Ensuring Patient Safety and Comfort
The secret to good dental visits for people with epilepsy is what happens ahead of time. A bit of planning before your appointment really pays off in comfort, safety, and peace of mind.
Comprehensive Medical History Intake
Start with a full talk—by yourself, your loved one, or your dental team—covering:
- Seizure type and frequency: When was your last seizure? What sets them off? How often do they happen?
- Medications: Which epilepsy drugs do you take, and when?
- Other health issues: Any other problems, allergies, or times in the hospital?
- Emergency contact info: Who should the dental staff call if needed?
Don’t be shy. The more your dentist knows, the better they’ll look out for you.
Effective Communication with the Patient and Caregivers
If you’re there as a caretaker or support person, come ready to answer questions. Talking things through builds trust and keeps everyone on the same team.
Tip for dental pros: Talk slowly and use simple words. Ask questions that need more than a yes or no, and make sure the person understands you—this helps cut stress, which can trigger seizures.
Consultation with the Patient’s Neurologist
Unsure? Call the patient’s brain doctor. Ask for input if:
- Seizures aren’t under control
- The patient just changed meds
- You plan on using a lot of anesthesia or heavy sedation
Better together—everyone knows what to expect, and you’re not left guessing about extra steps.
Risk Assessment and Tailored Treatment Planning
Each person is different. Some might just need a cleaning, while others—especially those with a lot of seizures—need a more careful plan.
Work together on a treatment plan that fits the patient’s needs. Schedule shorter and calmer visits, usually earlier in the day when seizures are less common. Be ready to make changes if the patient’s health is different at the time of the visit.
Anxiety Management and Sedation Considerations
Worry is normal before seeing the dentist, but for people with epilepsy, it’s often even more. Fear can bring on a seizure—so fighting stress is really important.
- Try deep breaths, soft music, and gentle lights.
- Ask about light sedation: Mild calming medicine (given by a trained dentist or someone skilled) may help. Laughing gas (nitrous oxide) is usually safe and works well for a lot of people.
- Be careful: Extra calming medicine needs to be checked with the medical team, especially for complex health problems.
- Book appointments when the patient isn’t tired or hungry, often in the morning.
During the Appointment: Proactive Management and Prevention Strategies
Now you’re at the clinic—it’s all about little steps that help everyone succeed.
Creating a Stress-Free and Calming Dental Environment
Small comforts count. Picture a quiet, warm room. Short wait times. Friendly workers who use your name and know your needs. Some dental offices play soft music, offer heavy blankets, or use dim lights.
A nice hello, some patience, and a smile really help lower stress.
Optimal Patient Positioning in the Dental Chair
This is important: Always set up the dental chair so the person can recover fast if something happens. Slightly leaning back (not flat) is safest. This lowers the chance of falls if a seizure happens, and makes it easy to help with breathing.
Keep the armrests down and clear stuff away from the chair.
Safe Use of Local Anesthesia (Considerations for Vasoconstrictors)
Local numbing shots are usually fine for people with epilepsy. Some shots have stuff like epinephrine that may react with certain epilepsy medicines or cause a racing heart, which can bring anxiety.
Let your dentist know about all your meds. They’ll pick what’s safest for you.
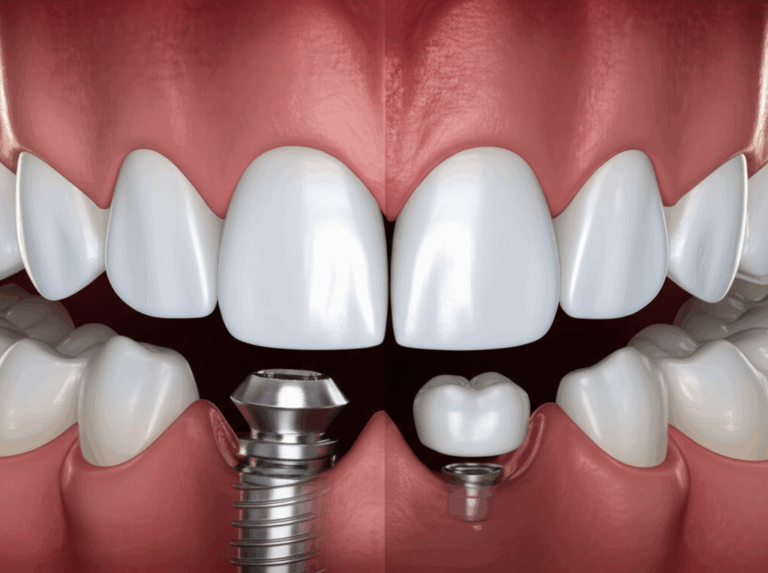
Preventing Dental Trauma During Potential Seizures
No one wants to think about a seizure at the dentist, but getting ready beats being surprised. Here’s how the team keeps you safe:
- Mouth props or bite blocks: Help prevent accidental biting of your tongue or the dentist’s tools.
- Never put fingers in the mouth: Always use tools, never bare hands, if you have to open someone’s mouth.
- Padded chair and tidy area: Keep tools out of the way and sharps locked up.
These simple acts are your safety net if anything goes wrong.
Continuous Patient Monitoring Throughout the Procedure
Dental workers will watch closely for any early signs of trouble. Sometimes people get a warning feeling before a seizure (called an “aura”). If you feel one, let the team know right away!
The team watches for little changes in breathing, how your eyes move, or muscle tension. Don’t ever feel bad about asking to pause or needing a break.
Managing a Seizure in the Dental Clinic: Emergency Protocol
Seizures rarely happen in dental offices, but every team should know what to do. If there’s a seizure, keep calm. A clear plan helps everyone.
Recognizing the Onset of a Seizure: Early Signs and Symptoms
Common warning signs:
- Blank stare or suddenly not reacting
- Jerky shaking or twitching, especially on one side
- Person may smell, taste, or feel something odd
- Sudden stiffening or collapse
If you see any, stop the dental work and move to safety steps.
Step-by-Step First Aid During a Tonic-Clonic Seizure
1. Clear the Area
Move anything sharp or breakable away from the patient. Guide the person gently if possible to keep them from hitting stuff.
2. Protect the Head and Airway (Don’t Hold Them Down)
Put something soft, like a towel or jacket, under the person’s head. Roll them to their side if possible to help with breathing and stop choking.
Never grab or hold someone down during a seizure—this can hurt them.
3. Time the Seizure
Most seizures last less than two minutes. It may seem longer. Watch the clock—timing matters for getting help.
4. Don’t Put Anything in the Mouth
Never put your fingers, tools, or anything else into someone’s mouth during a seizure. It won’t help and could cause harm.
Post-Seizure Care: Recovery Position, Monitoring, and Reassurance
Once the shaking ends, roll the person onto their side—the “recovery position.” This helps them breathe and clear out spit or vomit. Stay with them and talk quietly. They might be confused or sleepy for a while.
Watch over them until they’re fully awake. Don’t give food or drink until you’re sure they can swallow okay.
When to Call Emergency Medical Help
Get help right away if:
- The seizure lasts more than 5 minutes
- Another seizure follows right after
- The person doesn’t wake up soon
- They get badly hurt (broken bone, head injury, deep cuts)
- They have trouble breathing or it’s their first seizure ever
It’s always best to be careful—you can’t go wrong calling for help if you’re unsure.
Essential Emergency Kit Contents for Seizure Management
Every dental office that treats epilepsy patients should have a basic emergency kit:
- Oxygen and a way to give it
- Suction tool to clear spit or vomit
- Emergency medicine (only if the doctor says it’s okay—usually midazolam or diazepam)
- Gloves, towels, and emergency phone numbers
Check your kit often to make sure everything works.
Post-Appointment Care and Long-Term Oral Health Management
Dental care keeps going even after you leave the office. Good habits and check-ins help prevent more problems down the line.
Providing Clear and Simple Post-Treatment Instructions
After your visit, your team should explain what to do next in easy steps. If you have epilepsy—whether you’re the patient or caretaker—written notes can help remind you of what’s needed.
If you had sedation or small surgery, ask about eating, medicines, and warning signs to watch for.
Teaching Good Daily Mouth Care
Taking care of your mouth each day matters a lot. Here’s what helps people with epilepsy:
- Soft toothbrush or electric brush: Makes brushing easier if you have shaky hands.
- Fluoride toothpaste: Helps stop cavities.
- Antibacterial mouth rinse: Good for fighting gum problems, especially if you have overgrown gums.
- Special tools: Long-handled brushes or floss holders can help if your hands don’t work well.
Setting Up Regular Checkup Visits
Routine dental visits aren’t just for when you have a toothache. For people with epilepsy, checkups and cleanings every 3–6 months help find small problems before they get big.
Make your visit schedule fit your needs. Some folks need more visits for a while to get things back on track.
Handling Oral Side Effects
If your gums get thick and puffy (gum overgrowth), your dentist might suggest:
- Better brushing and flossing: Doing this more often can reduce buildup.
- Professional cleanings: Targeting the swollen areas.
- Medicine review: Your dentist and brain doctor can talk; sometimes changing drugs helps fix gum swelling.
- Surgery: In tough cases, a dentist can trim back extra gum tissue.
Other problems—like dry mouth or mouth sores—need their own care. Saliva substitutes, sugar-free gum, or special mouth rinses can help.
Staff Training and Clinic Preparedness: Building a Confident Team
Great care means the whole dental team needs to be ready for any surprise.
Regular Practice and Drills on Seizure Response
Practicing what to do in an emergency is really important. Dental teams should review the plan at least twice a year and run through pretend situations.
What to review:
- How to spot early warning signs
- Where emergency gear is kept
- What steps to take, one by one
- What to do after an event
Making and Sharing Simple Emergency Rules
Clear written steps make tough moments easier. List who calls for help, who stays with the patient, and where supplies are kept.
Keep these posted in staff rooms so no one forgets.
Keeping Emergency Equipment Ready to Go
That emergency kit only helps if it’s full and working. Pick someone to check the supplies every month and swap out anything old.
Test suction, oxygen, and medicine spots during drills. You want everything close and ready if you ever need it.
Teamwork Rules
Dental care is best when patient, caregivers, doctors, and all dental staff work together.
Being a team leads to better care, smoother visits, and more confidence for everyone.
Conclusion: Prioritizing Safety, Compassion, and Comprehensive Dental Care
Facing the idea of a seizure at the dentist can make anyone nervous. But with planning, simple steps, and a caring dental team, dental visits can be safe and much less stressful.
What to Remember
- Dental care and epilepsy work together: With the right steps and open talk, seizures in the dental office are uncommon and can be handled well.
- Medicines matter: Watch for side effects like sore gums or dry mouth—fix them early with your dental team’s help.
- Plan ahead: Tell your history, lower stress, and see a dentist who gets your needs.
- Emergency plans help: Dental offices must be ready, and so should you—know your triggers, meds, and who to call if you need help.
- Speak up!: Tell your dentist what you need, ask questions, and take charge of your health.
Ready? Book a talk with your dentist (or help your loved one do it). Bring this guide or your own questions and make a plan together for safe care.
Interested in more about special dental treatments? A china dental lab can create custom dental solutions for all kinds of needs.
Curious about new ways dentistry uses technology? Check out a digital dental lab for faster, easier procedures—great for people who want less time in the chair.
And if grinding at night is a worry after a seizure, a night guard dental lab can make you a custom product to keep your teeth safe.
Every smile deserves great care, no matter what health challenges you face. Let’s keep your smile happy, healthy, and safe—one smart step at a time!
Sources
- Centers for Disease Control and Prevention (CDC): Epilepsy Data and Statistics
- World Health Organization (WHO): Epilepsy Factsheet
- American Dental Association (ADA): Oral Health Topics: Epilepsy
- Special Care Dentistry Association: Guidelines for Dental Management of Patients with Neurologic Disorders
- Dental research articles about treating people with epilepsy, available on PubMed and in professional dental journals
Remember: This article is for information only and can’t replace advice from your doctor or dentist. Always talk to a professional when unsure.