A Comprehensive Clinical Guide to Dental Traumatology: Diagnosis, Management, and Prognosis
Table of Contents
Introduction to Dental Traumatology
The first time I saw dental trauma in real life, I was surprised how fast an accident could mess up a mouth – or even change how someone feels about themself. Dental trauma is any hurt to teeth, gums, or the bone around the teeth because of a fall, hit, or other accident. It can happen when kids fall on a playground, sports players bump into each other, or someone falls down the stairs.
The numbers are pretty shocking too. Studies say nearly 1 out of every 3 kids will have a dental injury before they grow up. It happens to adults too. In my work, I’ve seen all kinds of problems – a small chip, a big crack, or even a tooth fully knocked out.
Why is this so serious? If you help fast and treat it right, you can often save the tooth for a long time. If you wait too long or do things wrong, it’s much more likely to lead to pain, infection, or the tooth being lost forever. This guide is written to help you get comfortable and ready so you’ll know just what to do when a dental injury happens.
Classification and Diagnosis of Dental Traumatic Injuries
Clinical Examination Protocol
The first thing I learned in dental trauma is don’t rush. Take your time to figure out what’s going on. When someone comes in, I always start by asking what happened. How did they get hurt? How long ago? Did they stay awake? What did they do with the tooth if it got knocked out? Small details matter and can change what you do next. Also, I ask about pain, swelling, sensitivity, and bleeding.
Then I check if anything else got hurt. Sometimes the jaw, face, or even the head gets injured too – you need to make sure there’s no concussion or major problems. After that, I look inside the mouth. I check the teeth, gums, and how the teeth meet when the person bites. I use cold spray or a pulp tester to see if the tooth is still alive, especially if it looks bad.
Radiographic Examination
Taking good x-rays is really important in dental trauma. Usually I get small close-ups (periapical), top or bottom views (occlusal), and side views if needed. If it’s a bigger mess or lots of teeth are hurt, a 3D scan (cone beam CT) can show more. The extra info makes the next steps much easier to plan.
IADT Classification of Dental Trauma
Knowing the type of injury is super important since the treatment can be very different. I use the International Association of Dental Traumatology (IADT) system – it’s simple but covers everything. Here’s what I look for:
- Injuries to Hard Dental Tissues and Pulp
- Enamel fracture: just chipped outer cover.
- Enamel-dentin fracture: deeper chip into the next layer.
- Complicated fractures: the nerve inside the tooth gets hurt.
- Crown-root and root fractures: the break goes under the gum or into the root.
- Injuries to Periodontal Tissues
- Concussion: tooth isn’t loose but it hurts.
- Subluxation: a little loose but didn’t move out of place.
- Luxation: tooth moved – out, to the side, or jammed in.
- Avulsion: tooth knocked out all the way.
- Injuries to Supporting Bone
- Alveolar process fractures: bone around the tooth is broken.
- Injuries to Oral Soft Tissues
- Cuts, tears, or bruising on the lips, gums, or inside the mouth.
Knowing exactly what kind of injury you’re dealing with helps you plan what comes next and makes it easier to talk with other doctors or family.
Emergency Management and First Aid Protocols
Helping with dental trauma often starts before a dentist even sees the patient. I’ve had parents show up with a tooth in a plastic bag, water, or wrapped in a tissue – sometimes doing more hurt than help. With a tooth that’s been knocked out, every minute counts.
Some simple things I always tell people:
- Stay calm. Panic just makes everything harder.
- If a tooth is knocked out: Touch only the top part of the tooth (the white crown). If it’s dirty, rinse quickly with milk, saline, or a special tooth-saving solution. Don’t use plain water. If you can, put the tooth back in the socket right away (I’ve talked parents through this on the phone) – but this is only for adult teeth, never baby teeth.
- Don’t scrub the root – that damages the cells the tooth needs.
- If you can’t put it back, store it in milk or saline, never in water or dry tissues.
Once the patient comes in, I stop the pain, manage bleeding, and check if they need a tetanus shot. I numb the area if needed, sometimes give antibiotics, and clean the area really carefully. If a tooth is out of place or broken, I gently move it back and use a soft wire or plastic to hold it steady for a while.
For cuts or wounds in the mouth, it’s important to clean out all dirt or tooth pieces – miss one, and you might have a problem later.
Quick and smart action matters a lot in dental trauma. Working with a skilled dental ceramics lab or a crown and bridge lab is also very useful for fixing up broken teeth fast and making sure they look good.
Clinical Management of Specific Dental Traumatic Injuries (Permanent Teeth)
Crown Fractures
Small, simple chips need smoothing and maybe some polish. If the chip goes deeper into the tooth, I use bonding (composite) to fill and fix the look. If I can find the broken piece, I often glue it back on – it makes the tooth look normal again and helps the patient feel better, especially kids. If the inside nerve is showing, I try to cover it to keep the tooth alive, especially in young people.
Crown-Root Fractures
These can be tough. If the break is just above the gum or bone, I fix it directly. If it’s deeper, it may need a small surgery, or sometimes the tooth can’t be saved.
Root Fractures
These are very serious. I keep the tooth still with a splint and check again over months. Some root breaks close to the end of the root heal better than those closer to the gum.
Concussion & Subluxation
If the tooth hurts or is a bit loose but hasn’t moved, I tell patients to eat soft food, rest, and come back for check-ups. Even if it looks okay, it can develop problems later on – so I keep watching.
Luxation Injuries
If the tooth is out of place or jammed, I gently put it back and put on a soft splint for a few weeks. At every visit, I check if the tooth is still alive.
Avulsion
A tooth that’s knocked out is an emergency. Put it back as fast as possible, splint it, give antibiotics if needed, and watch closely for signs of failure. How long the tooth is out and where it was stored makes a huge difference. Milk or a proper tooth preservation solution work the best.
Alveolar Process Fractures
When the bone around the tooth is broken, you have to put it back just right and use a firmer splint. If it’s bad, sometimes a surgeon needs to help.
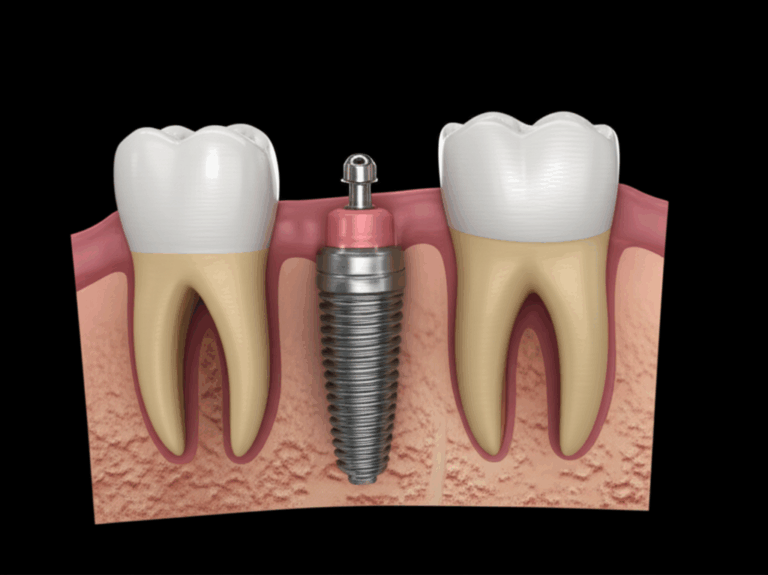
If the tooth can’t be saved, a fake tooth or denture made by a removable denture lab can help bring back a normal look and chewing.
Management of Traumatic Dental Injuries in Primary Dentition
Helping small kids with baby teeth is always hard. You have to be extra careful because you don’t want to hurt the grown-up teeth underneath.
If it’s a small chip on a baby tooth, I just fix it simple. If the nerve is showing, sometimes I do a small nerve procedure, or remove the tooth if needed. If the baby tooth is just a little loose but not moved, mostly I just watch it and tell the kid to eat soft foods. If it’s a big move or got knocked out, usually I pull the tooth – putting it back in can hurt the future grown-up tooth. With children, you always have to think of how their jaws and bite will grow.
Follow-up and Long-Term Prognosis
Dental trauma is usually not a one-and-done appointment. Good notes and regular checkups are super important. I see people back at 1 week, 1 month, 3 months, 6 months, and then every year – sometimes for up to five years. At every visit, I look for loose teeth, pain, color changes, or any signs the tooth or bone is having problems.
Common Complications
Stuff I look out for:
- Pulp death: tooth dies and may need a root canal.
- Root resorption: root starts melting away or gets stuck to bone (ankylosis).
- Pulp canal closes up: tooth turns dark or yellow.
- Looks or bites not right: tooth doesn’t look normal or can’t be used for chewing.
Prognostic Factors
How things work out depends on the kind of injury, how bad it is, how fast the tooth got fixed, how it was stored (if it came out), the patient’s age, and how well the person follows directions after. Teaching people (including parents and kids) about mouthguards and what to do if it happens again is also super important for prevention.
Interdisciplinary Approach and Advanced Topics
Dental trauma often needs a team. My best results happen when endodontists (root canal experts), orthodontists (braces), prosthodontists (tooth makers), and oral surgeons all help together.
For looks, sometimes a simple white filling works, and other times we need strong fake teeth made out of stuff like zirconia or e.max by a special digital dental lab to get a perfect match.
New treatments for kids with open roots (regenerative endodontics) can sometimes heal a tooth that would’ve been lost before, which is really great. Also, I keep really good notes and follow the rules, just in case there’s any legal trouble.
Finally, stopping injuries before they happen is best – mouthguards for sports, safety rules at schools, and simple reminders make a huge difference. A little bit of prevention can save a ton of trouble.
Conclusion
After all these years working with dental trauma, I see there’s a lot to learn, and every accident teaches something new. Fast help, good diagnosis, following steps, and caring about the person, not just the tooth – that’s what matters. When you face a dental injury, stay calm, follow the plan, use your resources, and listen to the patient. Every smile you save is worth every bit of effort.
If you’re curious to learn more about how labs can help with fixing teeth and making them look just right, you can check out china dental lab or the crown and bridge lab. Working closely with great lab teams really helps my patients and makes the results so much better.
Dental trauma care is about more than just teeth – it’s about making people feel whole and confident again. It’s a job worth doing well, and I’m happy to share what I know.